Aerosol/Droplet Expiration
Studies have confirmed that COVID-19 RNA is transported by aerosol, but no study has confirmed infection via aerosolized SARS-CoV-2 virus.
High level of certainty:
- Humans produce aerosols by expiratory activities: breathing, speaking, coughing, and sneezing1,2.
- Humans expire aerosols at generally 10-1 to 100 cm-3 in a range of particle sizes both larger and smaller than in diameter3–5. The mass and volume of expired materials is dominated by droplets (>5 µm; a size threshold defined by the infectious disease community6) whereas the number is dominated by aerosols (<5 ).
- Infectious pathogens (e.g. 4) are known to be carried in aerosol form by natural expiratory activities including breathing7.
Low level of certainty:
- Dominant mechanisms for aerosol formation:
- vibration of the vocal folds of the larynx where voice loudness may increase the total volume and mass of particles produced8;
- opening of occlusions in the small airways of the lungs (“fluid film burst”) 9,10;
- airflow turbulence in the respiratory tract interacting with fluids lining the walls of the airways11;
- droplets from the mouth produced during speech or coughing5.
- The number concentration and size distributions from healthy or infected adults producing aerosols during expiratory activities (e.g. breathing, speaking, coughing, sneezing)5,8 has been studied by a number of groups, but low concentrations of expiration, correction for dilution and variations due to relative humidity contribute to uncertainty in the measurements.
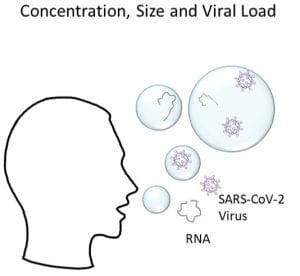
- Viral loading as a function of size of aerosol for different pathogens ()7 are still uncertain for many viruses and conclusions for one virus do not necessarily translate to other viruses. Samples of influenza in exhaled breath resulted in geometric mean RNA copy numbers of 3.8 × 104/30-minutes for aerosols (< 5 µm) and 1.2 × 104/30-minutes for droplets (> 5 µm) compared with 8.2 × 108 per naso-pharyngeal swab7.
- Variability in particle or aerosol expiration among healthy or sick individuals is not well quantified and models using expiration should note uncertainty in the variability of expiration source terms.
Unknown:
- Current studies have been unable to conclusively determine whether viable SARS-CoV-2 virons are aerosolized during expiratory activities (e.g. breathing12, speaking, coughing, sneezing).
- The rates of SARS-CoV-2 release within droplets and aerosols for different expiratory activities (e.g. breathing, speaking, coughing, sneezing) has yet to be quantitatively measured.
- Pathogen loading in the aerosols produced and pathogen loading as a function of size of aerosol.
* The statements above are intended to be reviewed regularly as more information and new references emerge. If you have queries about the content of the above and wish to discuss these please contact the editors.
References:
- Duguid, J. P. The size and the duration of air-carriage of respiratory droplets and droplet-nuclei. J. Hyg. (Lond). 44, 471–479 (1946).
- Papineni, R. S. & Rosenthal, F. S. The size distribution of droplets in the exhaled breath of healthy human subjects. J. Aerosol Med. Depos. Clear. Eff. Lung 10, 105–116 (1997).
- Gralton, J., Tovey, E., McLaws, M. L. & Rawlinson, W. D. The role of particle size in aerosolised pathogen transmission: A review. J. Infect. 62, 1–13 (2011).
- Fennelly, K. P. Particle sizes of infectious aerosols: implications for infection control. Lancet. Respir. Med. 2600, 1–11 (2020).
- Johnson, G. R. et al. Modality of human expired aerosol size distributions. J. Aerosol Sci. 42, 839–851 (2011).
- Chartier, Y and Pessoa-Silva, C. Natural ventilation for infection control in health-care settings. (World Health Organization, 2009).
- Yan, J. et al. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc. Natl. Acad. Sci. U. S. A. 115, 1081–1086 (2018).
- Asadi, S. et al. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 9, (2019).
- Johnson, G. R. & Morawska, L. The mechanism of breath aerosol formation. J. Aerosol Med. Pulm. Drug Deliv. 22, 229–237 (2009).
- Malashenko, A., Tsuda, A. & Haber, S. Propagation and breakup of liquid menisci and aerosol generation in small airways. J. Aerosol Med. Pulm. Drug Deliv. 22, 341–353 (2009).
- Moriarty, J. A. & Grotberg, J. B. a Mucus – Serous Bilayer. J. Fluid Mech. 397, 1–22 (1999).
- Ma, J. et al. Exhaled breath is a significant source of SARS-CoV-2 emission. medRxiv 2020.05.31.20115154 (2020). doi:10.1101/2020.05.31.20115154